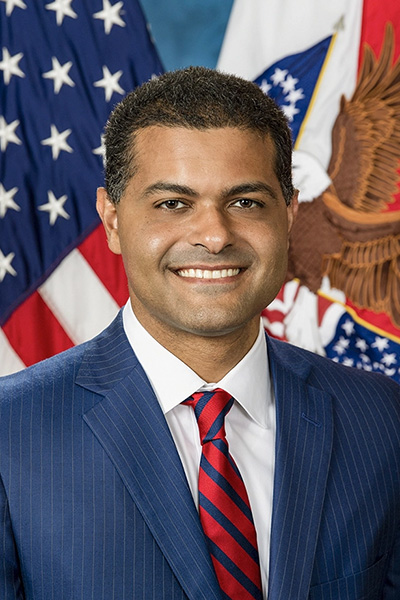
Meet Dr. Shereef Elnahal, Undersecretary for Health
Congratulations on your confirmation as the Under Secretary for Health at VA. In this role, you lead the Veterans Health Administration (VHA), the largest integrated health care system in the United States, which oversees the delivery of care to more than nine million enrolled veterans. As we head into the 2023, what issues do you believe should be prioritized to improve care and support for veterans?
It’s my honor to serve America’s Veterans as the Under Secretary for Health. When I took on this role, I established six priorities for system-wide improvement on behalf of the 9 million enrolled veterans we serve and those we hope to serve in the future. I consider them our most important strategic and operational goals.
- Hire faster and more competitively.
- Connect Veterans to the soonest and best care.
- Serve Veterans with toxic exposures.
- Accelerate our journey to High Reliability.
- Support Veterans’ whole health, their caregivers, and survivors.
- Prevent Veteran suicide.
These aren’t just words on a page. For those of us in VHA, they provide the framework for all we do. On this frame, we are building out programs to create a highly effective, responsive organization for the nation’s Veterans. To enable us to meet these strategic priorities, we will work to retain, invest in, and support our workforce. We will respect and honor the diversity among our employees and Veterans. That is our strength. We’ll seek to continually improve our technology, encourage innovation, and modernize our facilities. We also want to enhance our partnerships with federal and state agencies, NGOs, and community organizations. This unity will strengthen our fight against Veteran suicide and our efforts to reach Veterans where they are.
According to WWP’s 2022 Annual Warrior Survey, over 9 out of 10 WWP Alumni are enrolled in VA health care, but most of America’s veterans are not. Why should veterans choose VA, and how can WWP Alumni spread that message?
VA is the largest health care system in the country and is recognized, year after year, for providing quality health care and services. Veterans regularly give VA high marks in customer satisfaction surveys and our clinicians are regarded as among the leaders in the country’s health care community and in health research. Most importantly, no other health care system is entirely devoted to providing a lifetime of health care to Veterans and to their overall whole health and well-being. To put it simply, VA knows and understands the Veteran experience and Veterans’ needs. You’ve earned this care as a Veteran. You deserve it. We in VA are entirely and exclusively dedicated to you.
You previously served as the Assistant Deputy Under Secretary for Health for Quality, Safety, and Value at VA from 2016 through 2018. During that time, you co-founded the VHA Innovation Ecosystem, a program which fosters the spread of innovation and best practices to improve care for veterans. Can you tell us about what inspired you to co-found this program, and some of the ways that this program has developed and cultivated innovation at VA?
We founded the VHA Innovation Ecosystem with a simple hypothesis: that the employees closest to the Veteran know what needs to be done to improve the care we provide to Veterans. We realized VHA needed to create more opportunities to empower our clinicians and administrators to create positive change and decided to empower our front line and teams closest to the Veteran with the power to do so. We sought to improve our capacity to recognize promising innovation when it was occurring, make more intentional investments in those areas, and ultimately deliver the benefits to all Veterans.
VHA Innovation Ecosystem creates value through investment in our frontline employees whom we believe are our greatest asset for delivering innovative solutions to VHA’s most pressing health care challenges. For example, through our Spark-Seed-Spread investment program, we focus on bridging the “possibilities gap.” This has led VHA team members to pioneer transformative capabilities such as our Office of Advanced Manufacturing and VA Rideshare.
Additionally, the VHA Diffusion of Excellence (DoE) plays a complementary role by replicating and scaling innovations and promising practices across our nationwide system through an annual Shark Tank competition. To date, VHA DoE has replicated 90 Shark Tank winners over 1,000-plus times and scaled 14 national solutions across the VA health care system.
On August 10, the Honoring our PACT Act (P.L. 117-168) became law. This comprehensive new law regarding toxic exposure is the largest expansion of health care and benefits in VA history. What steps is your office taking to welcome veterans who are newly eligible for care at VHA facilities and what actions should veterans to take to access their new VA benefits?
On outreach to veterans who could benefit from the PACT Act, we are working every day to ensure that there is no wrong door for veterans to access VA care. Our Veterans Experience Office has mapped the veteran engagement journey across all possible touch points with veterans. Whether a veteran or survivor comes to VA through a medical center, a benefits office, a website, or any other way, we are ensuring that veterans receive information about these new benefits. This is especially important for our post-9/11 combat veterans, many of whom qualify for the one-year special enrollment period that began on October 1, 2022. As we near the final six months of that eligibility window, we want to get as many veterans enrolled in VA health care as possible.
As soon as the Senate sent the bill to the President’s desk, we launched va.gov/pact, a one-stop shop website for understanding the PACT Act and applying for benefits. We also enhanced 1-800-My-VA-411, an easy to remember telephonic front door for veterans and their supporters with 24/7 live agents.
We are reaching out to veterans directly through their communities and local VA medical centers. During the week of December 10th, we hosted 127 PACT Act “Week of Action” events in all 50 States, the District of Columbia, and Puerto Rico, to do targeted outreach, including claims clinics, health care enrollment, and toxic exposure screenings. Additionally, we’re reaching out to over 370,000 participants in our burn pit registry through email, regular mail, and social media. We’re also sending direct mail and email communications to more than 1.1 million eligible but not-enrolled Veterans, inviting them to learn more about their possible eligibility and enroll.
We have implemented a nationwide effort to screen veterans who already get care from us to determine potential toxic exposures. As of March 7, we have screened nearly 2.3 million veterans, with 42 percent reporting exposures. As of November 8th, this is a routine part of care in every medical center in the country. And it allows us to refer veterans directly to VBA as they may qualify for enhanced benefits, or an increase in their priority group.
Mental health remains a top priority for Wounded Warrior Project. What mental health initiatives are you most focused on in the coming year?
 VA continues the fight to break down the negative stigma associated with mental health conditions and other barriers that may keep Veterans from getting the care they need and deserve. We will be releasing an updated version of the handbook that spells out the mental health services each facility is required to provide. Our comprehensive national policy outlines the continuum of mental health care: peer support and self-help apps; mental health care integrated within primary care and specialty medicine; outpatient treatment and specialized services for those with trauma, specialized, intensive treatment programs for addiction and those at risk for suicide; and acute inpatient, emergency, and residential treatment. Providing this full continuum of mental health care services ensures Veterans have access to the level and type of care they need when they need it.
VA continues the fight to break down the negative stigma associated with mental health conditions and other barriers that may keep Veterans from getting the care they need and deserve. We will be releasing an updated version of the handbook that spells out the mental health services each facility is required to provide. Our comprehensive national policy outlines the continuum of mental health care: peer support and self-help apps; mental health care integrated within primary care and specialty medicine; outpatient treatment and specialized services for those with trauma, specialized, intensive treatment programs for addiction and those at risk for suicide; and acute inpatient, emergency, and residential treatment. Providing this full continuum of mental health care services ensures Veterans have access to the level and type of care they need when they need it.
We will continue to increase virtual care options and make them more accessible, offering telemental health, as clinically appropriate, to all Veterans. We will be focusing on hiring, particularly for providers for Veterans with substance use disorders, as we face a national opioid epidemic. We will undertake an in-depth examination of access and utilization of VA mental health services by demographic groups and conduct an analysis of health inequities to assist our facilities in addressing identified disparities.
Suicide prevention continues to be a top priority for us and is woven into care across mental health and beyond. We will continue to focus on the public health model, advancing efforts to reach Veterans in clinical settings and in the community. We are training providers in new evidence-based treatments for suicide prevention and we are setting up hubs of providers who can provide these services virtually to increase access. We are also partnering with many community organizations to provide grants and support for suicide prevention work, and we have expanded eligibility to enrolled and nonenrolled eligible Veterans to receive emergent suicide care at no cost.
These are only a few of the many things we will be doing this year. I hope it conveys the overall reality that we cannot focus on mental health without addressing a Veteran’s whole health. Our approach to mental health care addresses each Veteran as a unique individual and in advancing methods that empower and equip them to achieve their life goals.
WWP’s 2022 Annual Warrior Survey showed that 89.3% of warriors who were offered a telehealth appointment chose to use telehealth at some point during the previous year. How do you see telehealth evolving in the future and how do you see it improving the quality of care that is available to veterans?
Telehealth is a core part of VA’s mission to connect Veterans to care from anywhere in the U.S. It is one of many essential tools in our clinicians’ tool belts for care in VA and should be viewed as such. It is many times an appropriate and more timely option for care, while not as appropriate in other circumstances. Veterans and clinicians should make the decision about telehealth together, and specific to individual Veterans’ needs. We’ve seen the benefits of telehealth during the past three years, when it has grown tremendously. Last year, over 2.3 million Veterans used telehealth as part of their VA care — totaling over 11 million episodes of care.
Telehealth has made care much more accessible and convenient for many Veterans because they can connect with their VA providers from where they are. They don’t have to go to a VA facility, which can be time-consuming, costly, or physically taxing in the case of Veterans with disabilities. If a Veteran lives somewhere without readily accessible specialty care, they can use telehealth to consult with a VA specialist that may live hundreds of miles away. Further, many Veterans prefer the comfort and convenience of accessing care from home, particularly for mental health appointments.
We also recognize that many Veterans face barriers to accessing telehealth care. VA is dedicating resources to bridging some of these barriers. For example, through the Digital Divide Consult, VA is helping Veterans who don’t have internet access or don’t have a working computer or mobile device. The Digital Divide Consult is a process that connects those Veterans with programs that can provide free or discounted internet service, mobile devices, and phone service. These services can enable those Veterans to access telehealth care.
In the future, we envision a VA health system without walls — that will continue to expand care options beyond the clinic to include easily accessible virtual care options. We want to give all Veterans the option to use telehealth care when appropriate, including more specialty care options.




 Kirsten Laha-Walsh, the first ever HillVets-WWP fellow, who provided exceptional support for veteran mental health and caregiver advocacy.
Kirsten Laha-Walsh, the first ever HillVets-WWP fellow, who provided exceptional support for veteran mental health and caregiver advocacy. James Anderson, Director of Veterans Engagement with the Office of Public Engagement at the White House, whose efforts supported WWP in many ways, including making the 2022 WWP Soldier Ride DC so successful.
James Anderson, Director of Veterans Engagement with the Office of Public Engagement at the White House, whose efforts supported WWP in many ways, including making the 2022 WWP Soldier Ride DC so successful.

 Health Care and Benefits: On August 10, President Biden signed the
Health Care and Benefits: On August 10, President Biden signed the  Clothing Allowance: Another significant accomplishment included within the Consolidated Appropriations Act of 2023 was the language of the
Clothing Allowance: Another significant accomplishment included within the Consolidated Appropriations Act of 2023 was the language of the  Adaptive Vehicles, Military Spouse Hiring, Self-employment: We also saw progress in several other areas surrounding veterans’ financial security. The
Adaptive Vehicles, Military Spouse Hiring, Self-employment: We also saw progress in several other areas surrounding veterans’ financial security. The 











 What did you hope to accomplish during the fly-in, and do you feel you’ve accomplished that goal?
What did you hope to accomplish during the fly-in, and do you feel you’ve accomplished that goal? Was there a specific topic or piece of legislation you wanted to advocate for during this trip? If so, what was it, and do you feel the members/staff were receptive to your thoughts?
Was there a specific topic or piece of legislation you wanted to advocate for during this trip? If so, what was it, and do you feel the members/staff were receptive to your thoughts? Prior to Operation Advocacy, would you have considered advocating for legislation on your own?
Prior to Operation Advocacy, would you have considered advocating for legislation on your own? What did you hope to accomplish during the fly-in, and do you feel you’ve accomplished that goal?
What did you hope to accomplish during the fly-in, and do you feel you’ve accomplished that goal? Were you looking to take away any skills from this experience? If so, what were they, and did you apply them in your interactions with Members/staff?
Were you looking to take away any skills from this experience? If so, what were they, and did you apply them in your interactions with Members/staff? Has this experience inspired you to go home and advocate for veteran-friendly legislation at your state and local level?
Has this experience inspired you to go home and advocate for veteran-friendly legislation at your state and local level?
 We actually met in College Station where he was stationed, and we had mutual friends from church. I was at church, and he was at church, and we went to lunch together and that’s how we met. Ours was what you would consider a non-traditional love story, meeting somebody in your late 40s; we both had families and adult children from previous marriages, and things are just very different when you approach dating from that point in your life. So, we started seeing each other, but he was in the reserves and six months after we started dating, he was unexpectedly deployed to Kuwait to replace an officer who ended up getting sick.
We actually met in College Station where he was stationed, and we had mutual friends from church. I was at church, and he was at church, and we went to lunch together and that’s how we met. Ours was what you would consider a non-traditional love story, meeting somebody in your late 40s; we both had families and adult children from previous marriages, and things are just very different when you approach dating from that point in your life. So, we started seeing each other, but he was in the reserves and six months after we started dating, he was unexpectedly deployed to Kuwait to replace an officer who ended up getting sick.
 Rich lost his courageous battle with cancer almost exactly a year after the Major Richard Star Act was first introduced in February of 2020 by Rep. Bilirakis and Rep. Ruiz. Since you started this journey, what moments have impacted you the most?
Rich lost his courageous battle with cancer almost exactly a year after the Major Richard Star Act was first introduced in February of 2020 by Rep. Bilirakis and Rep. Ruiz. Since you started this journey, what moments have impacted you the most? In March, Wounded Warrior Project flew in warriors from all over the country to advocate for legislation that would benefit post-9/11 veterans. What would you like to say to the warrior alumni who came to Washington, DC, to advocate for the Major Richard Star Act?
In March, Wounded Warrior Project flew in warriors from all over the country to advocate for legislation that would benefit post-9/11 veterans. What would you like to say to the warrior alumni who came to Washington, DC, to advocate for the Major Richard Star Act?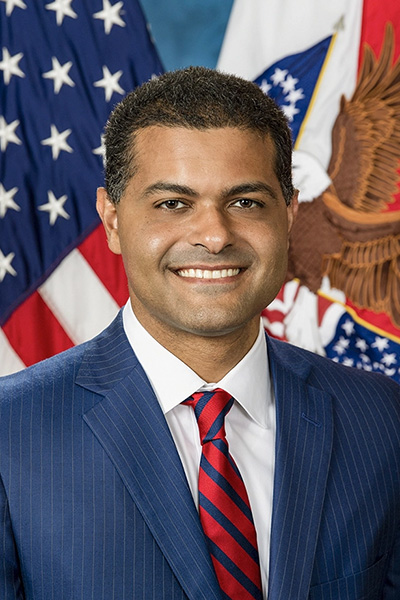
 VA continues the fight to break down the negative stigma associated with mental health conditions and other barriers that may keep Veterans from getting the care they need and deserve. We will be releasing an updated version of the handbook that spells out the mental health services each facility is required to provide. Our comprehensive national policy outlines the continuum of mental health care: peer support and self-help apps; mental health care integrated within primary care and specialty medicine; outpatient treatment and specialized services for those with trauma, specialized, intensive treatment programs for addiction and those at risk for suicide; and acute inpatient, emergency, and residential treatment. Providing this full continuum of mental health care services ensures Veterans have access to the level and type of care they need when they need it.
VA continues the fight to break down the negative stigma associated with mental health conditions and other barriers that may keep Veterans from getting the care they need and deserve. We will be releasing an updated version of the handbook that spells out the mental health services each facility is required to provide. Our comprehensive national policy outlines the continuum of mental health care: peer support and self-help apps; mental health care integrated within primary care and specialty medicine; outpatient treatment and specialized services for those with trauma, specialized, intensive treatment programs for addiction and those at risk for suicide; and acute inpatient, emergency, and residential treatment. Providing this full continuum of mental health care services ensures Veterans have access to the level and type of care they need when they need it. As of January 1, 2023, the Department of Veterans Affairs (VA) is processing all related claims under the
As of January 1, 2023, the Department of Veterans Affairs (VA) is processing all related claims under the 